|
Absorption (skin)Skin absorption is a route by which substances can enter the body through the skin. Along with inhalation, ingestion and injection, dermal absorption is a route of exposure for toxic substances and route of administration for medication. Absorption of substances through the skin depends on a number of factors, the most important of which are concentration, duration of contact, solubility of medication, and physical condition of the skin and part of the body exposed. Skin (percutaneous, dermal) absorption is the transport of chemicals from the outer surface of the skin both into the skin and into circulation. Skin absorption relates to the degree of exposure to and possible effect of a substance which may enter the body through the skin. Human skin comes into contact with many agents intentionally and unintentionally. Skin absorption can occur from occupational, environmental, or consumer skin exposure to chemicals, cosmetics, or pharmaceutical products. Some chemicals can be absorbed in enough quantity to cause detrimental systemic effects. Skin disease (dermatitis) is considered one of the most common occupational diseases.[1] In order to assess if a chemical can be a risk of either causing dermatitis or other more systemic effects and how that risk may be reduced, one must know the extent to which it is absorbed. Thus, dermal exposure is a key aspect of human health risk assessment. Factors influencing absorptionAlong with inhalation, ingestion and injection, dermal absorption is a route of exposure for bioactive substances including medications.[2] Absorption of substances through the skin depends on a number of factors:
In general, the rate of absorption of chemicals through skin follows the following scheme from fastest to slowest: Scrotal > Forehead > Armpit ≥ Scalp > Back = Abdomen > Palm = under surface of the foot.[4] Structures influencing absorptionTo be absorbed through the skin, a chemical must pass through the epidermis, glands, or hair follicles. Sweat glands and hair follicles make up about 0.1 to 1.0 percent of the total skin surface.[2] Though small amounts of chemicals may enter the body rapidly through the glands or hair follicles, they are primarily absorbed through the epidermis. Chemicals must pass through the seven cell layers of epidermis before entering the dermis where they can enter the blood stream or lymph and circulate to other areas of the body. Toxins and toxicants can move through the layers by passive diffusion. The stratum corneum is the outermost layer of the epidermis and the rate-limiting barrier in absorption of an agent.[4] Thus, how quickly something passes through this thicker outer layer determines the overall absorption. The stratum corneum is primarily composed of lipophilic cholesterol, cholesterol esters and ceramides. Thus lipid-soluble chemicals make it through the layer and into the circulation faster, however nearly all molecules penetrate it to some minimal degree.[5][6] Absorption of chemicals in municipal water and dental products such as VOC (Volatile Organic Compounds), TTHM (Total Trihalomethanes), fluoride and disinfectants is a major exposure to environmental health hazards.[7][8][9] 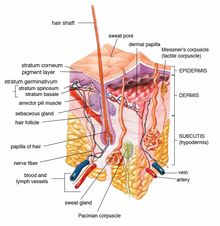 Conditions affecting skin absorptionAgents that injure the stratum corneum, such as strong acids, are absorbed faster than chemicals that do not.[10] Skin damage due to burns, abrasions, wounds and skin diseases also increase absorption. Thus populations with skin damage may be more susceptible to adverse effects of agents that are absorbed through the skin. Certain solvents like dimethyl sulfoxide (DMSO) act as carriers and are frequently used to transport medication through the skin. DMSO increases the permeability of the stratum corneum.[11][12] Surfactants like sodium lauryl-sulfate increase the skin penetration of water-soluble substances, possibly by increasing the skin permeability of water.[11] Medical use of skin absorptionDermal application of a medication or chemical allows treatment to be localized, unlike ingestion or injection. Some medications seem to be more effective (or are more efficient) using the dermal route of administration. Some ingested drugs are heavily metabolized by the liver and may be inactivated, but using a dermal application bypasses this metabolic step allowing more parent compounds to enter the peripheral circulation. If a drug is absorbed well through the skin it may be used as a means of systemic medication. Dermal dosage forms include: liniments, braces, lotions, ointments, creams, dusting powders, aerosols, and transdermal patches.[13] Specially designed patches are currently used to deliver fentanyl, nicotine and other compounds. Slower skin absorption versus oral or injectable may allow patches to provide medication for 1 to 7 days.[14] For instance nitroglycerin given transdermally may provide hours of protection against angina whereas the duration of effect sublingually may only be minutes.[15] Measurement of skin absorptionThe amount of chemical that is absorbed through the skin can be measured directly or indirectly.[16] Studies have shown there are species with differences in the absorption of different chemicals. Measurements in rats, rabbits or pigs may or may not reflect human absorption.[10] Finding the rate at which agents penetrate the skin is important for assessing the risk from exposures. Direct measurementIn vivoThe transit of chemicals into the skin can be directly measured using non-invasive optical techniques with molecular specificity, such as Confocal Raman Spectroscopy. This technique is able to identify unique spectra of molecules and compare to background skin spectra whilst limiting measurement regions using confocal gating, achieving depth-resolved concentration measurement. A single measurement sequence can thereby establish a snapshot profile of chemical concentration against depth inside the skin. By repeating the measurement at multiple timepoints, a dynamic concentration-at-depth profile is determined. Since modern Raman Spectrometers exhibit extremely high SNR, in-vivo absorption testing in human skin is possible on a scale of a few minutes or hours. A chemical may also be directly applied to the skin followed by blood and urine measurements, at set time points after the application, to assess the amount of chemical that entered the body. The concentration in the blood or urine at particular time points can be graphed to show an area under the curve and the extent and duration of absorption and distribution to provide a measure of systemic absorption. This can be done in animals or humans with a dry chemical powder or a chemical in solution.[17] Rats are commonly used for these experiments. An area of skin is shaved before the chemical is applied. Often the area of chemical application is covered to prevent ingestion or rubbing off of the test material. Samples of blood and urine are taken at specific time intervals following application (0.5, 1, 2, 4, 10, and 24 hours) and in some protocols at the chosen end time the animal maybe necropsied. Tissue samples may also be evaluated for the presence of the test chemical.[18] In some test protocols many animals may be tested and necropsies may occur at set intervals after exposure. Biomonitoring, such as taking urine samples at intervals, from workers exposed to chemicals may provide some information but it is difficult to distinguish dermal from inhalation exposure using this method. Ex vivoThe permeability properties of the stratum corneum are, for the most part, unchanged after its removal from the body.[18] Skin that has been removed carefully from animals may also be used to see the extent of local penetration by putting it in a chamber and applying the chemical on one side and then measuring the amount of chemical that gets into a fluid on the other side.[14] One example of this ex vivo technique is the isolated perfused porcine flap.[4] This method was first described in 1986 as a humane alternative to in vivo animal testing.[19] In vitroTechniques such as static diffusion cells (Franz cells) and flow-through diffusion cells (Bronaugh cells) have also been used.[4] The Franz Cell apparatus consists of two chambers separated by a membrane of animal or human skin. Human skin is preferred but due to ethical and other considerations is not always available. Human skin often may come from autopsies or plastic surgeries.[20] The test product is applied to the membrane via the top chamber. The bottom chamber contains fluid from which samples are taken at regular intervals for analysis to determine the amount of active cells that has permeated the membrane at set time points. Bronaugh cells are similar to Franz cells but use a flow-through system beneath the membrane layer and samples of the liquid below are taken continuously rather than at set time points.[21] Bronaugh cells have been replaced with inline cells by some manufacturers. Indirect measurementIt is sometimes impossible for humane reasons to apply a drug to the skin and measure its absorption. Sarin, a nerve gas, can be absorbed through intact skin and be lethal at low concentrations. Thus if one needs to assess the risk of Sarin exposure one must take skin absorption and other routes into account but one cannot ethically test Sarin on human subjects; thus ways of modeling the risk from skin exposure of the agent have been found. Models are used in some instances to predict the amount of exposure or absorption and to assess public health hazards. In order to assess the risk of a chemical causing a health issue one must assess the chemical and the exposure. Exposure modeling depends on several factors and assumptions.
Skin contact with dry chemical
Skin contact with chemical in solution (water, etc.)
Skin contact with gas or aerosol
Controlling skin absorptionIf skin exposure and absorption are deemed to indicate a risk, various methods to reduce absorption can be undertaken.
See also
References
External links
|